Today I sent the following email to the Editor of New York Magazine:
As a reader of New York Magazine, I have come to expect your articles to be accurate, well-researched, and fair. Unfortunately your recent piece, “Has Long COVID Always Existed?” by Jeff Wise is none of these things. As someone familiar with the topics covered, I can tell you that the article is misleading, biased, and riddled with errors. Worse, it exacerbates longstanding misconceptions that people with ME/CFS and Long COVID must overcome when seeking effective care, and it risks reviving myths about this condition that I and many others have worked for decades to dispel.
I have personal experience with ME/CFS and its consequences. I was an Ivy League-educated attorney when I got sick with ME/CFS almost thirty years ago, and I have spent more than two decades advocating for scientific research into the disease. For the past ten years, I have covered issues and developments in the ME/CFS community on my blog, Occupy ME. My work has also been published by the Philadelphia Inquirer, STATNews, and on Psychology Today.
I find the bias and inaccuracies in Mr. Wise’s article especially surprising and discouraging given that his previous reporting, including on Paxlovid and Omicron, has been accurate, balanced, and reasonable. Those articles relied on solid research and experts in the field and fulfilled the journalistic goal of helping readers understand complex topics.
Sadly, Mr. Wise’s most recent article stands in sharp contrast to those previous pieces in terms of both quality and accuracy. Instead of investigating the science of Long COVID and seeking to help readers understand the possible origins and nature of the condition, Mr. Wise seems to simply promote his own views of the illness. Time and again, he reinforces the myth that Long COVID is a psychiatric disorder treatable with exercise and therapy. He presents a biased view of the state of the science on Long COVID and ME/CFS that is not supported by the evidence, as many journalists and experts have already pointed out. (See Putrino, Davenport, O’Rourke, Tufecki, #MEAction, Tuller)
Throughout the article, Mr. Wise used selective quotation, vague or inaccurate descriptions, incomplete or misleading statements, and biased sources to convince readers of his conclusion that Long COVID is merely “the latest manifestation of an endemic psychiatric condition.” I wish to draw your attention to three specific instances where Mr. Wise misused source material in support of his argument.
1.Mr. Wise grossly mischaracterized the finding of a Harvard University study into the relationship between psychological distress and the risk of developing Long COVID.
Building on previous studies suggesting that mental distress can be associated with longer and more severe respiratory infections, the Harvard researchers sought to examine associations between psychological distress and Long COVID. They surveyed participants for self-reported psychological distress at the beginning of the study, and then monitored them for over a year to determine how many reported having COVID and/or post-COVID symptoms. Analysis of the data showed that people who reported pre-infection symptoms of depression, anxiety, worry about COVID, loneliness and perceived stress were more likely to report Long COVID symptoms, and those with high levels of two or more types of distress were at nearly 50% greater risk of Long COVID symptoms.
Mr. Wise reported this factual finding of the paper, but he then remarked that some patients might reject idea that Long COVID is a psychiatric condition, implying that the paper’s results prove that this is the case. Indeed, his interpretation of this research is so wrong that it is almost as if he read the abstract but not the full text of the paper.
Most perplexing is Mr. Wise’s failure to mention that the study authors stated explicitly that Long COVID is not a psychiatric condition. The authors wrote, “Our results should not be misinterpreted as supporting a hypothesis that post-COVID-19 conditions are psychosomatic.” More than 40% of participants with Long COVID reported no pre-infection emotional distress. Symptoms of Long COVID differ substantially from symptoms of mental illness, and the correlation between pre-infection distress and Long COVID remained even when people reporting only psychiatric, cognitive, or neurological symptoms were excluded from the analysis.
Notably, the authors cite several papers that found, “more than 50% of patients with post-COVID-19 conditions report relapses triggered by physical activity. In contrast, physical activity is protective against relapse of mental illness.” This acknowledgement that patients did not improve with exercise but, in fact, worsened their condition is especially relevant given Mr. Wise’s contention that exercise is an effective treatment for the disease. Finally, the authors identified multiple biological factors that could explain why pre-infection emotional distress might increase the risk of developing Long COVID. They cite, for example, the link between distress and chronic systemic inflammation.
Ultimately, Mr. Wise took research that adds an important if nuanced dimension to our understanding of risk factors for Long COVID and distorted the finding to match his own conclusion that Long COVID is a psychiatric condition. The truth is that the authors of the study expressly rejected that conclusion in the discussion section of the paper. Mr. Wise fails to acknowledge any of that in his article, and as a result misleads the reader.
2.Mr. Wise selectively edited a quote from a paper in SN Comprehensive Clinical Medicine to overstate the authors’ conclusion.
For this study, doctors at the Mayo Clinic Florida reviewed and summarized published research on the characteristics and clinical management of Long COVID. The authors did not attempt a meta-analysis to quantitatively analyze the pooled data from the included papers. Rather, they synthesized and summarized the “narrative evidence” from 117 articles covering dozens of treatments across fifteen broad categories of symptoms and signs, including respiratory, cardiovascular, and neurologic complications.
Mr. Wise cited this paper as support for the use of CBT and exercise therapy as treatments at Long COVID clinics, writing, “This approach has been endorsed by researchers: Mayo Clinic researchers published a study in April that recommends treating chronic fatigue patients with ‘Cognitive Behavioral Therapy (CBT)…graded exercise, mindfulness, and sleep hygiene.’” However, the discussion of treating chronic fatigue is limited to four sentences in the Specialty Care section of the paper and one bullet point in Table 1. Mr. Wise edited the text from Table 1 to make it sound like a clear recommendation. A review of the full quote, however, shows that this is not the case. Here is the full quote with the deleted material italicized:
“Chronic fatigue: There is potential role for Cognitive Behavioral Therapy (CBT) and Health & Wellness Coaching (HWC) programs focused nutritional status, graded exercise, mindfulness, and sleep hygiene, with the goal of improved quality of life.”
This study did not “endorse” CBT and graded exercise as a treatment for Long COVID; it merely suggests a “potential role” for CBT and Health & Wellness coaching to “improve quality of life.” What’s more, Mr. Wise did not acknowledge, as the study authors did in the body of the paper, that, “There is a paucity of information on the management of patients with fatigue, myalgias, and exercise intolerance.”
Because of how Mr. Wise selectively edited that quote and failed to accurately describe the full context of the study, readers are led to the erroneous conclusion that the paper firmly established CBT and/or exercise as effective treatments for Long COVID. This false narrative can do real harm to people with Long COVID because, as the previous paper noted, the majority of them experience relapse after physical activity.
3.Finally, Mr. Wise unfairly and inaccurately portrayed the ME/CFS patient community as spiteful and extremist.
Throughout his article, Mr. Wise quoted blogs and blog comments without naming, citing, or linking to the comments themselves. As I reviewed and fact-checked his assertions, I was surprised to discover that one of those comments had been cherry-picked from my website (without attribution). Indeed, Mr. Wise omitted the context that contradicts the point he was making—that ME/CFS advocates are extremists who have undue influence on medical guidelines.
To help paint this picture of advocates consumed by vitriol, Mr. Wise devoted an entire paragraph to the conflict between the ME/CFS community and Dr. William Reeves from the Centers for Disease Control, even though that conflict ended with Dr. Reeves’ death more than ten years ago. This section of Mr. Wise’s article jumps around in time from 2015 to 2021, then back to 2012 for the Reeves discussion, before going forward again to 2013-2015, which must be confusing to readers not already familiar with the history. After stating that patients were “enraged” by Dr. Reeves’ claim that people with ME/CFS were mostly suffering from personality disorders, Mr. Wise wrote that Dr. Reeves’ death in 2012 “did little to assuage the community’s enmity.” He then quoted “one blog commenter” in support of that statement. In fact, the quote came from a comment someone posted on a blog post I wrote when Dr. Reeves died, but Mr. Wise took it out of context and misrepresented it as indicative of the opinion of the entire community.
When Dr. Reeves passed away, I wrote about some of his history with ME/CFS and my own impression from meeting him in person in 2006. I concluded with this statement: “And in the end, he was a man and not a caricature. He has often been viewed as disdainful of the suffering of people with CFS; we should not make the same mistake and be disdainful of the pain his family and friends must feel at his passing.” But obviously, my statement doesn’t match the impression Mr. Wise is trying to create, so he didn’t quote me. Instead, he presented as representative of the whole ME/CFS community a single comment posted on the blog by someone who “can not bring myself to have one ounce of any sympathy” because of all the suffering caused by Dr. Reeves’ influence on ME/CFS research.
Mr. Wise advances the idea that the community hated Dr. Reeves because that would support his portrait of advocates as self-absorbed extremists. He presented without context a single comment made on a blog post ten years ago, as if it reflected the views of millions of people in the ME/CFS community. It does not. There was disagreement, expressed on my blog and in the community as a whole, about the legacy of Dr. Reeves and how we should move forward. This is always the case in a community as large and diverse as people affected by ME/CFS.
Unfortunately, the complexity and nuance of the community does not appear to interest Mr. Wise. He presented only material that supports his view that advocates are extremists, and the misleading and selective way Mr. Wise quoted from my blog is just one example.
To be honest, I am surprised that the New York Magazine Intelligencer published this article in its current state. It reads more like a hit piece than journalism. I do not speculate as to Mr. Wise’s intentions. I can only say that this article is biased, misleading, and inflammatory. Mr. Wise misrepresented the state of the science on both ME/CFS and Long COVID, omitting all the evidence that contradicts his views. By publishing it, you have contributed to the misinformation about these diseases, and many people face potential harm as a result.
I understand that calls for corrections and even a retraction have been sent your way, and it is indeed important to correct the record. Beyond that, however, it’s clear that the issues of Long COVID and chronic illness are a growing concern for Americans, one that New York Magazine could play a leading role in addressing. As such, I would like to propose writing an article for your publication that would contribute to the public’s understanding of Long COVID, ME/CFS and other poorly understood chronic disease. If you are interested, I would be happy to share a summary of points I would cover.





Favorite Reads of 2023
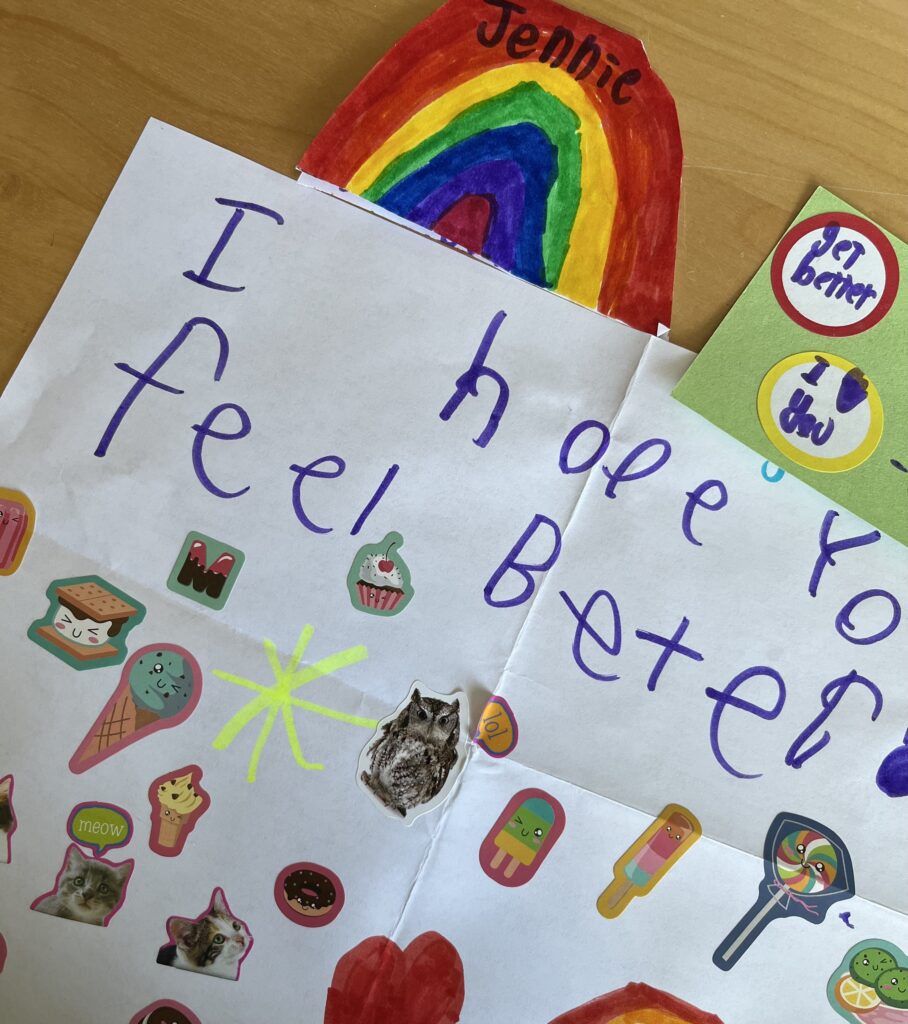
Listen, I know that everyone posted their favorite books of 2023 already. I wanted to as well, but my recovery from breast cancer surgery took longer than I anticipated, and now I’m getting radiation treatment. However, I still really want to share the books I loved last year, and since it’s still January, I think this is valid.
I’ve gotten more intentional about reading in the last few years. I used to just pick whatever book I felt like reading, without trying to hit a reading goal or focus on a specific list. I didn’t keep a book journal, so I tended to forget not only what happened in books I’ve read but even whether I had read them. Goodreads was great because at least I had a record of what books I read, but I deleted my account a couple years ago after one of the many review-bombing controversies.
I was inspired by the Reading Glasses podcast to try new ways of tracking my reading, and I ended up creating a personal database to help me manage my TBR (To Be Read) list and keep notes on what I loved (or didn’t). Don’t worry, I won’t inflict my nerdiness on you. All this is just to say that now I make more thoughtful choices about what to read. I don’t set specific goals or challenges for myself, but I don’t just choose books at random either.
I read fifty-six books in 2023, about the same as 2022. Interestingly, more of my 2023 favorites were fiction (unlike last year), and some of them were big chunky books. You’ll notice that I’m not into cozy mysteries or romance, but maybe there will be something in my list that appeals to you too.
Non-Fiction
Run Towards the Danger by Sarah Polley: I received this book as a gift, and I was skeptical at first because what did I have to learn from an Academy Award winning actor/screenwriter/director? I was wrong. Polley is a gifted writer, and this essay collection blew me away. The most compelling part to me was Polley’s description of her suffering and eventual recovery from a severe concussion. This book is inspirational without being glib, and Polley’s sincerity makes her writing feel like a personal conversation. I loved it.
Some of Us Just Fall by Polly Atkin: This memoir was published in the UK last year, but it looks like it will be available in the US in March. Atkin has Hypermobile Ehlers-Danlos syndrome and hemachromatosis, although it took many years for her to be properly diagnosed and treated. This memoir interweaves the experiences of being chronically ill with being in nature. Atkin lives in Grasmere, in England’s Lake District, the home of literary greats such as William Wordsworth, and still a place of incredible natural beauty. She brings us along on her walks and swims in a landscape that can heal some things but not everything, and shares her journey of learning to live well with her diagnoses.
Fiction
Six Deaths of the Saint by Alix Harrow: This is a short story, and I generally don’t read short stories, but this one is brilliant. I don’t even want to tell you anything about it and risk spoiling it for you. I will only say that when I got to the moment when the pieces of the story came together, I put my hand on my heart and gasped. Just trust me and read this.
Ordinary Monsters by J. M. Miro: This is a honker, and it is worth every minute it takes to read. If you like reading about dark academia, the grime of the Victorian era, magical mystery, and/or remarkable children, this book is for you. It’s the story of a shining boy, the people who love him, the people who want to use him, and the strength of found family. I got it from the library and ended up buying a copy because it is that good.
Yellowface by R.F. Kuang: I love everything by R.F. Kuang, and her novel Babel was one of my favorites last year. Yellowface is a completely different kind of book but equally amazing. The narrator steals her friend’s just finished manuscript and passes it off as her own work. As the story hurtles along, the characters grapple with racism, diversity, cultural appropriation, social media, and fame–or utterly fail to do so. Kuang is such a skillful writer that I found myself caring deeply for the narrator, despite the fact she’s a complete trainwreck who makes some very bad choices.
Starling House by Alix Harrow: Read this book if you like gothic mansions, small town secrets, a young woman discovering her strength, true love and sacrifice, and/or supernatural mysteries. Harrow’s first novel, The Ten Thousand Doors of January, is one of my favorite books of all time, and Starling House is pretty high on the list now, too.
The Last House on Needless Street by Catriona Ward: This is the first book I’ve read by Ward, and her entire backlist is now on my TBR. It’s described as a mystery/thriller, but it’s horror as well. Something very odd is going on in the creepy house on Needless Street, and a new neighbor wants to find the truth. The suspense kept yanking me forward, and there’s a solid twist that I did not see coming. Don’t read this if you are easily creeped out, but if you love psychological thrillers then definitely check it out.
Jonathan Strange and Mr. Norrell by Susanna Clarke: Most of my 2023 favorites were new releases, but this one is almost twenty years old. I read it around the time it came out and liked it, but I read it again in 2023 and LOVED it. The premise is that magic once existed in England, and now in the Napoleonic era, Strange and Norrell are trying to bring it back. They get more than they bargained for, with terrible consequences. Read this if you love the Regency period, myths and magic, faeries, and/or books with footnotes. Clarke is a quietly brilliant writer, and that didn’t really hit me until I finished the book.
Right now, I’m reading Demon Copperhead by Barbara Kingsolver, another chunky book by another brilliant author. I hope you’re reading something great, too!